Mapping Maternal Vulnerability: Insights to Drive Change

Health organizations increasingly need to understand where and why maternal vulnerability is greatest in the United States to develop interventions targeted to serve the most vulnerable populations and save lives. The rate at which women die from pregnancy-related issues in the US is double that of most other wealthy countries. For Black women, it is orders of magnitude higher. Reducing these deaths requires an understanding of the factors that make women vulnerable.
Healthcare for women has been a longstanding problem in the United States for numerous reasons including cost, access, insurance coverage, and state and federal policies. It is particularly problematic for low-income women and women of color.
The maternal mortality rate represents the number of women who die from pregnancy-related health issues or from health issues that were made worse because of pregnancy. In 2022, over 22 women died for every 100,000 live births. While this rate has dropped since last year, it remains double the rate of most other high-income countries. The maternal mortality rate for Black women was 49.5 deaths per 100,000 live births in 2022, which was significantly higher than the rates for White, Hispanic, and Asian women.
The Granular Maternal Vulnerability Index
The Granular U.S. Maternal Vulnerability Index (gMVI) from Surgo Health identifies where and why mothers in the US are vulnerable to poor maternal health outcomes and is now available to non-commercial subscribers of PolicyMap. Leverage it with other data in PolicyMap to strategically target areas where interventions or public policy initiatives could have the most impact.
Surgo’s gMVI ranks geographies on overall vulnerability to poor pregnancy outcomes and vulnerability across six themes: reproductive health, physical health, mental health and substance abuse, general healthcare, socioeconomic determinants, and physical environment. These six gMVI themes reflect 43 indicators associated with maternal health outcomes.
Reproductive Healthcare includes access to family planning and reproductive services including abortion, as well as availability of skilled attendants.
Physical Health status includes prevalence of noncommunicable diseases and sexually transmitted infections.
Mental Health and Substance Abuse include factors related to stress, mental illness, and addiction.
General Healthcare includes accessibility, affordability, and healthcare utilization, including insurance coverage and the state’s Medicaid expansion status.
Socio-economic Determinants of Health include educational attainment, poverty and food insecurity, and social support.
Physical Environmental factors that influence maternal health outcomes include violent crime rates, housing conditions, pollution, and access to transportation.
The overall index and those of the six themes are available at the state, county, zip code, and census tract level providing users with a very local view of the maternal health challenges facing women. The gMVI covers 50 U.S. states and the District of Columbia. The index is relative and ranks the vulnerability of U.S. geographic units against each other. The index ranges from 1 to 100 where a score of 100 indicates the worst vulnerability and 1 indicates the least vulnerability.
The Granular Maternal Vulnerability Index
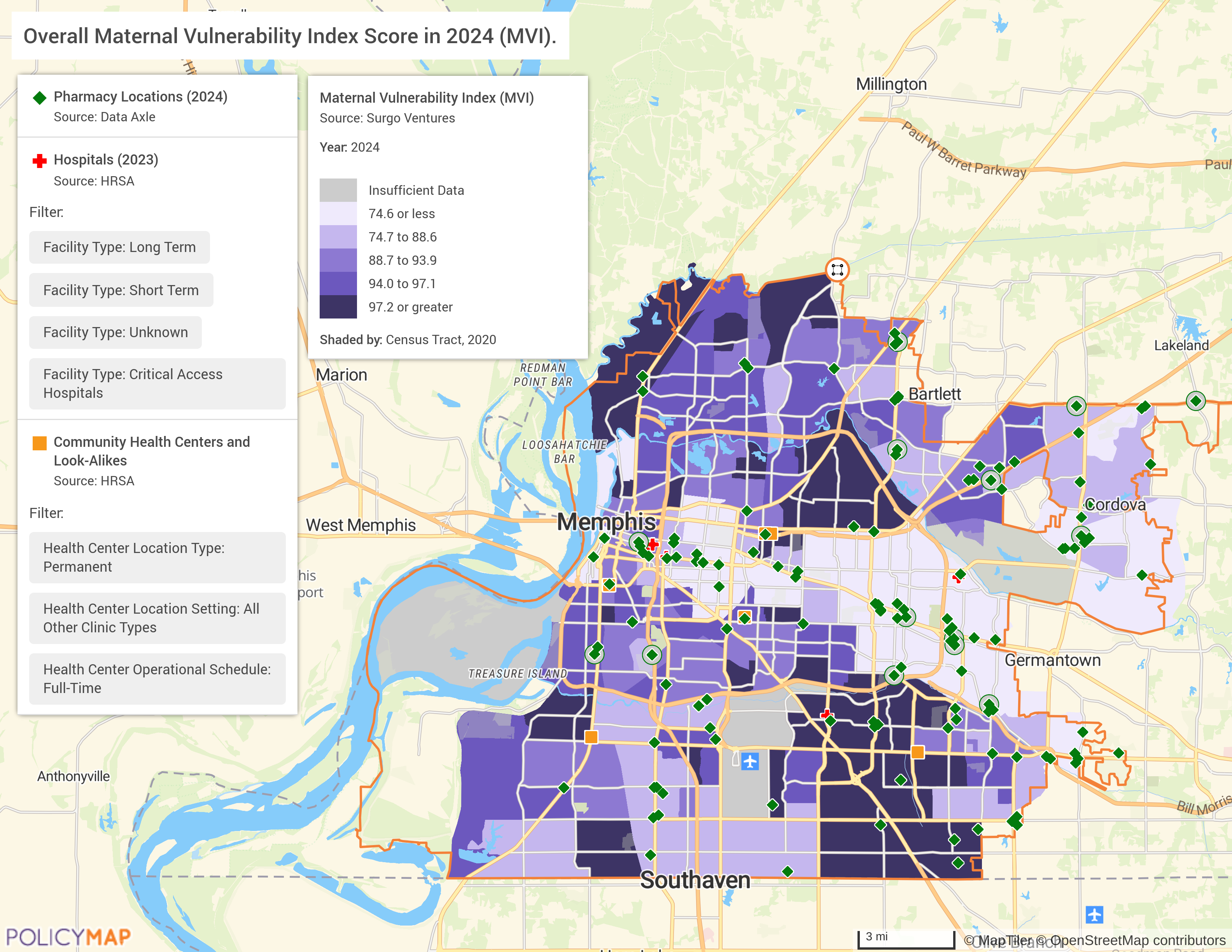
In Memphis, TN, for example, where abortion is banned, the risk level varies greatly between neighborhoods- ranging from a low of 22 in some neighborhoods to a high of 99.8 in others. In some places, such as the census tract called out below, the risk level is higher now than it was last year. Leveraging the gMVI along with PolicyMap data provides additional insights as to why and can foster the development of targeted interventions, such as increasing access to care, in areas where they are needed the most.

Access to care is seen as one of the primary means of improving maternal vulnerability. This includes, among others, access to hospitals, doctors, pharmacies, and transportation. Layering hospitals, full-time health care centers and pharmacies on top of the gMVI illustrates this in Memphis as areas with the least vulnerability, shown in the lightest purple on the map, have greater access to pharmacies, hospitals, and health centers than more vulnerable areas shaded in the darkest purple on the map.
Health organizations can use this information to zoom in on those places where interventions may be most needed. In Memphis, for example, organizations can pinpoint those neighborhoods with an gMVI of 95 or more and a Mental Health/Substance Abuse risk of 95 or more, to identify those neighborhoods where maternal vulnerability and mental health or substance abuse coincide. Those neighborhoods are shaded in the map below. Layering on mental health and substance abuse facilities enables organizations to see the precise location of available resources and prioritize interventions in areas where resources are needed but do not exist.

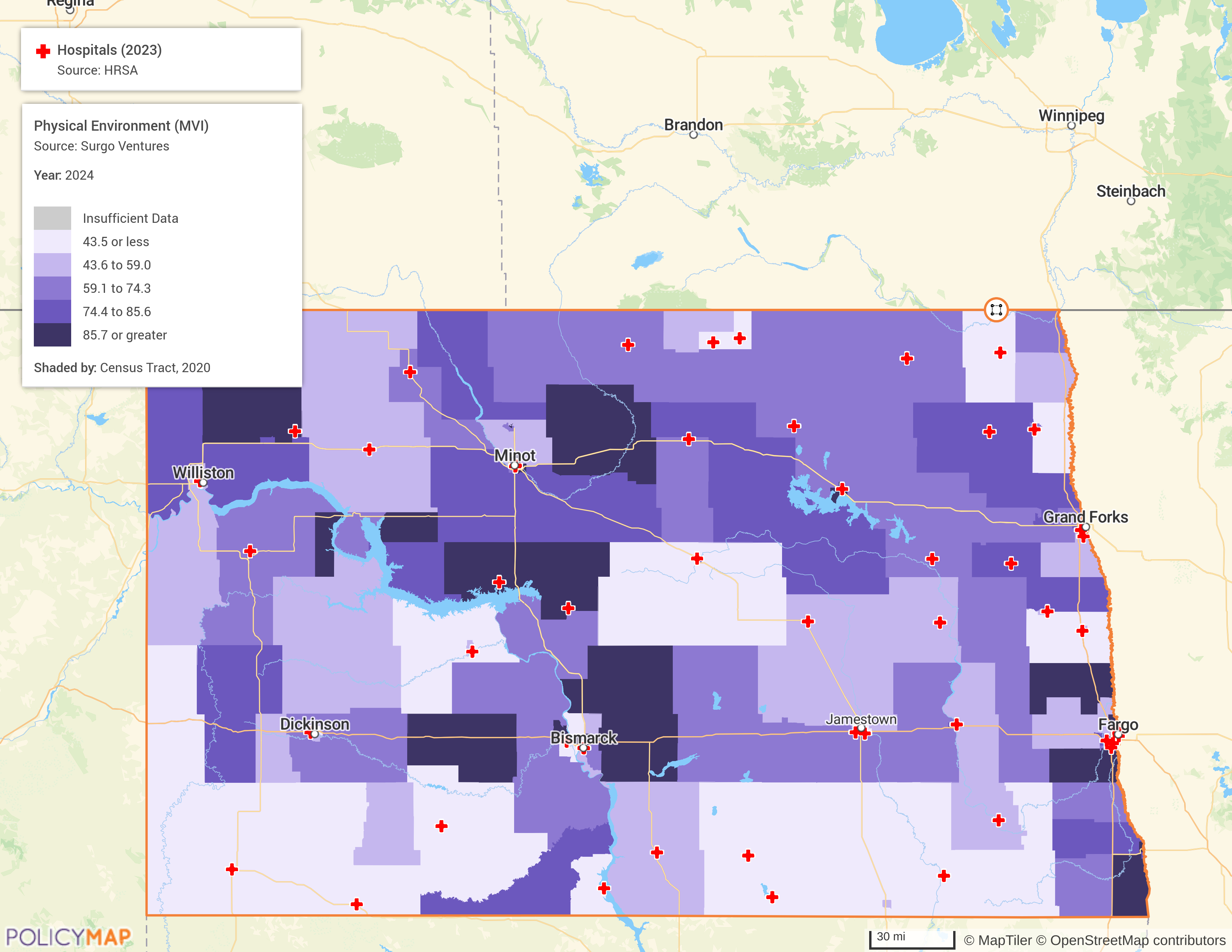
In rural areas, maternal vulnerability can also be tied to transportation access as getting to and from health provider locations or hospitals can be an insurmountable barrier. One of the gMVI themes available from Surgo in PolicyMap is Physical Environment which includes access to transportation as a barrier. In North Dakota, the darkest purple areas on the map are where women live who are most vulnerable to physical barriers, like a lack of access to transportation. Layering on Hospital locations pinpoints exactly where getting to a hospital presents a challenge and where interventions related to transportation may have the greatest impact.
Request More Information
Understanding where scarce resources can have the greatest impact becomes increasingly important as the roadmap for women’s health care in the United States seems more unpredictable than ever. Fill in the form below to request more information.