Food as Medicine: Dig Deeper into the Connection Between Nutrition and Health

Food as medicine (FaM) is capturing people’s attention across the United States, from the federal government to public health officials, large corporations, nonprofits, and venture capitalists. FaM is emerging as a dynamic, comprehensive approach to nutrition-based healthcare solutions. FaM models focus on providing food to support positive health outcomes through medically tailored meals or groceries, voucher-based food assistance, and prescriptions for produce.
Almost 60% of Americans report changed eating habits due to the pandemic and the rate of food-insecure households with children has grown significantly since 2020. FaM aims to address these consumption shifts and stressors by making healthy food more easily accessible to individuals and communities. In support of this, the 2022 White House Conference on Hunger, Nutrition, and Health led the federal government to set a goal of ending hunger and tackling diet-related diseases by 2030 through a substantial $8 billion federal investment in public and private-sector initiatives. The federal government allocated $2.5 billion to FaM start-up funding and the private sector invested an additional $1.8 billion in venture capital since 2022. These investments reflect a widespread commitment to advancing food security integrating nutrition into digital health strategies, and honing nutrition-centered disease prevention techniques.
Leveraging data-driven, geospatial insights on social determinants of health (SDOH)—such as heart disease prevalence, SNAP (Supplemental Nutrition Assistance Program) eligibility, and internet access—enables governments, non-profits, payers, and providers to ensure that nutrition-focused enterprises and initiatives effectively serve individuals and communities. PolicyMap can empower stakeholders to better understand the prevalence of food insecurity, nutritional distress, government assistance enrollment, and other critical determinants, in neighborhoods across the US. These insights can strategically drive targeted public and private sector investments.
The State of Food and Health in the US
The inextricable relationship between food and health is increasingly explained by the onset of public health initiatives, innovative products, and societal shifts toward an emphasis on nutrition-centered health. Studies show that more than 48 million U.S. households (60% of Americans) have a member with a health condition that can be managed by a nutrition-focused diet, representing $270 billion of all annual grocery sales.
Treating the prevalence of diet-related diseases costs approximately $1.1 trillion annually, equivalent to aggregate consumer grocery spending. Further, there are more than 350,000 annual deaths from cardiovascular disease linked to poor nutrition, contributing to total U.S. federal healthcare expenses approaching 20% of GDP. Thus, understanding the impact of nutrition intervention on population health has become crucial for public health initiatives and has proven to be an opportunity for growth in digital health spaces.
Although price is the primary consideration for many buyers, 84% of consumers still prioritize health and wellness when selecting fresh foods. Deloitte reports that three-quarters of consumers are now seeking personalized nutrition options: an increase of 13 percentage points compared to last year. Additionally, 55% of consumers are open to paying more for foods that enhance wellness.
While the impact of nutrition on health conditions varies widely, data show that medically-tailored-meals can improve health outcomes for conditions like chronic liver disease, HIV/AIDS, type 2 diabetes, and heart disease. Therapeutically nutritious meals are also linked to reduced healthcare utilization, spending, and mortality, especially for individuals with advanced heart failure. A 2022 study revealed that greater adoption of medically-tailored-meals for individuals with dietary conditions could prevent up to 1.6 million hospitalizations annually and save Medicare, Medicaid, and private payers a combined $13.6 billion per year.
Central to assessing the relationship between diet and health outcomes is understanding how social determinants play a role in access to information about nutrition, FaM programs, , and healthy food options. Determinants of population health, namely factors associated with community vitalization, environmental conditions, and resource accessibility, impact nearly 50% of Americans with diet-related diseases.
Food insecurity is particularly prevalent among Black households, with nearly 20% experiencing food insufficiency in 2021—more than double the 8% reported among white households. Black and Latino communities also face significantly higher average rates of diabetes and heart disease, which are linked to food insecurity and exacerbated by targeted advertising of unhealthy foods to youth. Furthermore, studies show that historic exclusionary policies have restricted access to stable employment, outdoor spaces, quality healthcare, and well-supported schools, further exacerbating disparities in access to nutritious foods.
The profound impact of nutrition on health highlights the necessity for public health strategies that address food insecurity and promote equitable access to healthy foods, encompassing the food as medicine approach. By focusing on social determinants and expanding access to nutrition-focused interventions, particularly for marginalized communities, governments, nonprofits, and payers can significantly reduce healthcare costs and improve population health.
Visualizing and Understanding Community-Level Needs
Understanding and visualizing community-level needs and social determinants of health is essential to implementing FaM interventions, as it enables stakeholders to address diet-related diseases, reduce healthcare costs, and enhance community health more effectively. Tools like PolicyMap provide crucial geospatial insights into food insecurity, nutritional challenges, and other key health indicators, allowing for better-targeted initiatives. By aligning resources with the specific needs of communities, FaM efforts will maximize impact and improve public health outcomes.
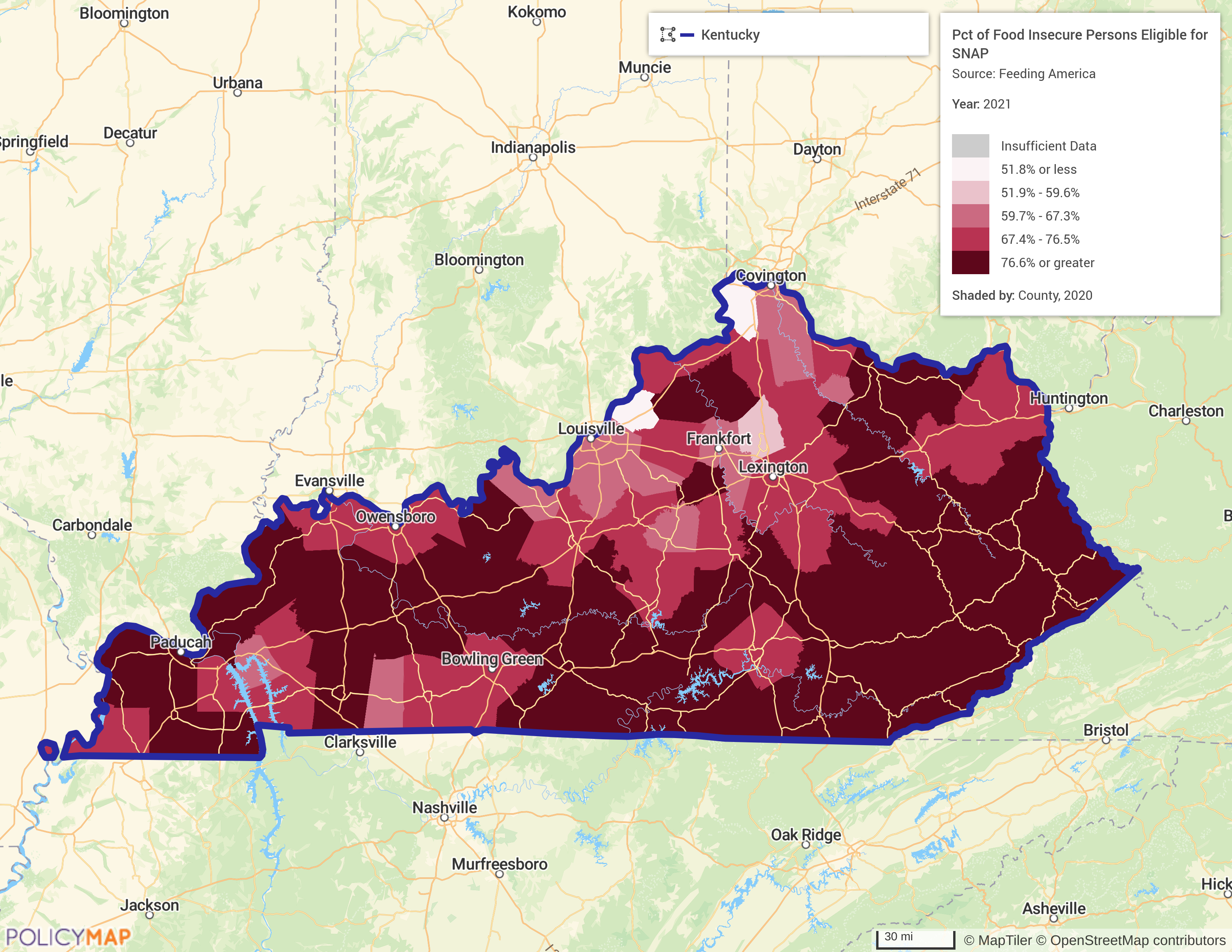
Leveraging existing programs like SNAP and WIC (Special Supplemental Nutrition Program for Women, Infants, and Children) will be critical for governments to expand coverage and initiatives to incorporate benefits into consumer-based deliverables. The map below, generated from the PolicyMap platform, shows the percentage of people per county in Kentucky who are eligible for SNAP.
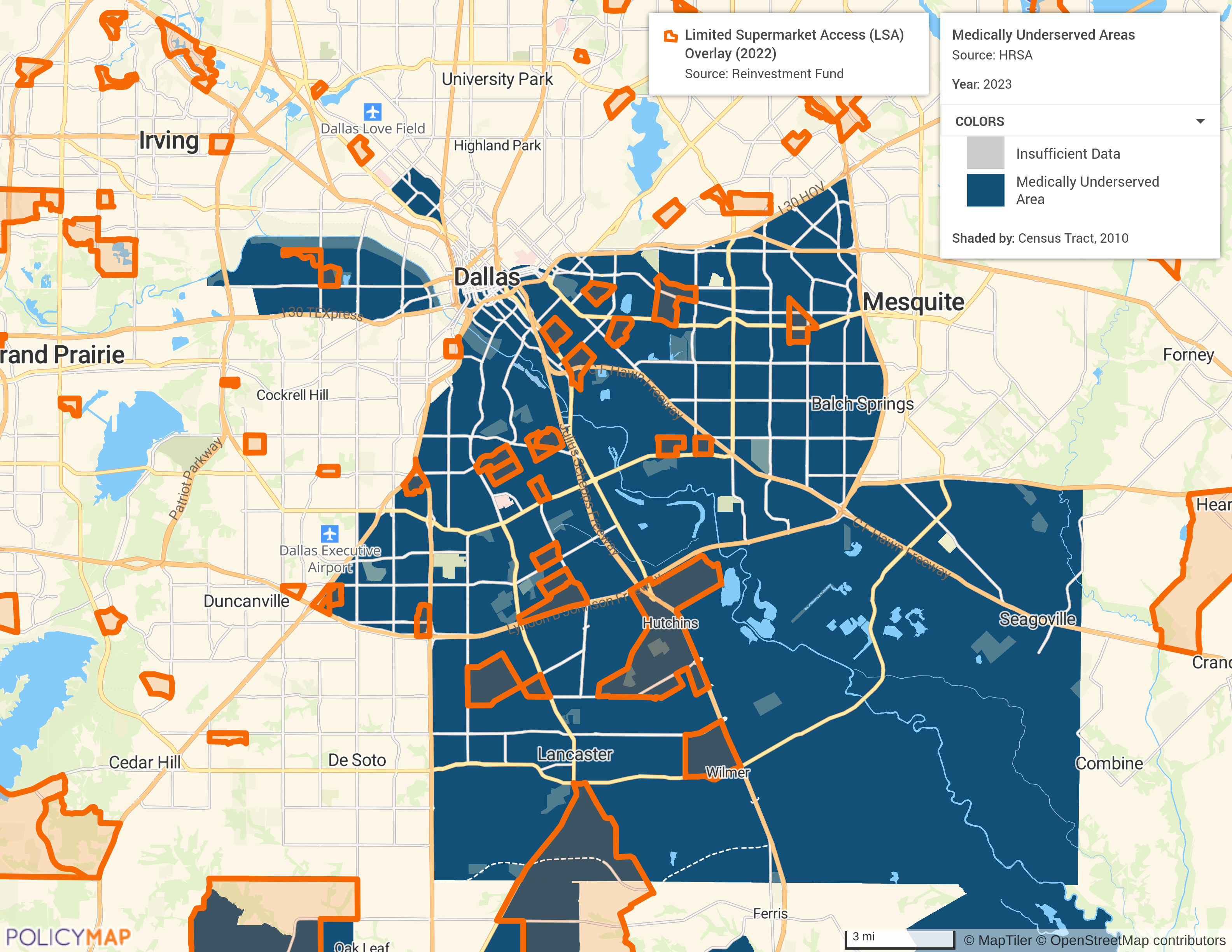
PolicyMap’s platform also enables users to derive insights on a variety of data points at a more granular level. Visualizing data at the census tract level and employing tools like Reinvestment Fund’s Limited Supermarket Access can show where people have limited food access (orange polygons) in medically underserved areas in, for example, Dallas (shaded blue). This can very quickly identify communities where the integration of nutrition and healthcare interventions would have a significant impact.
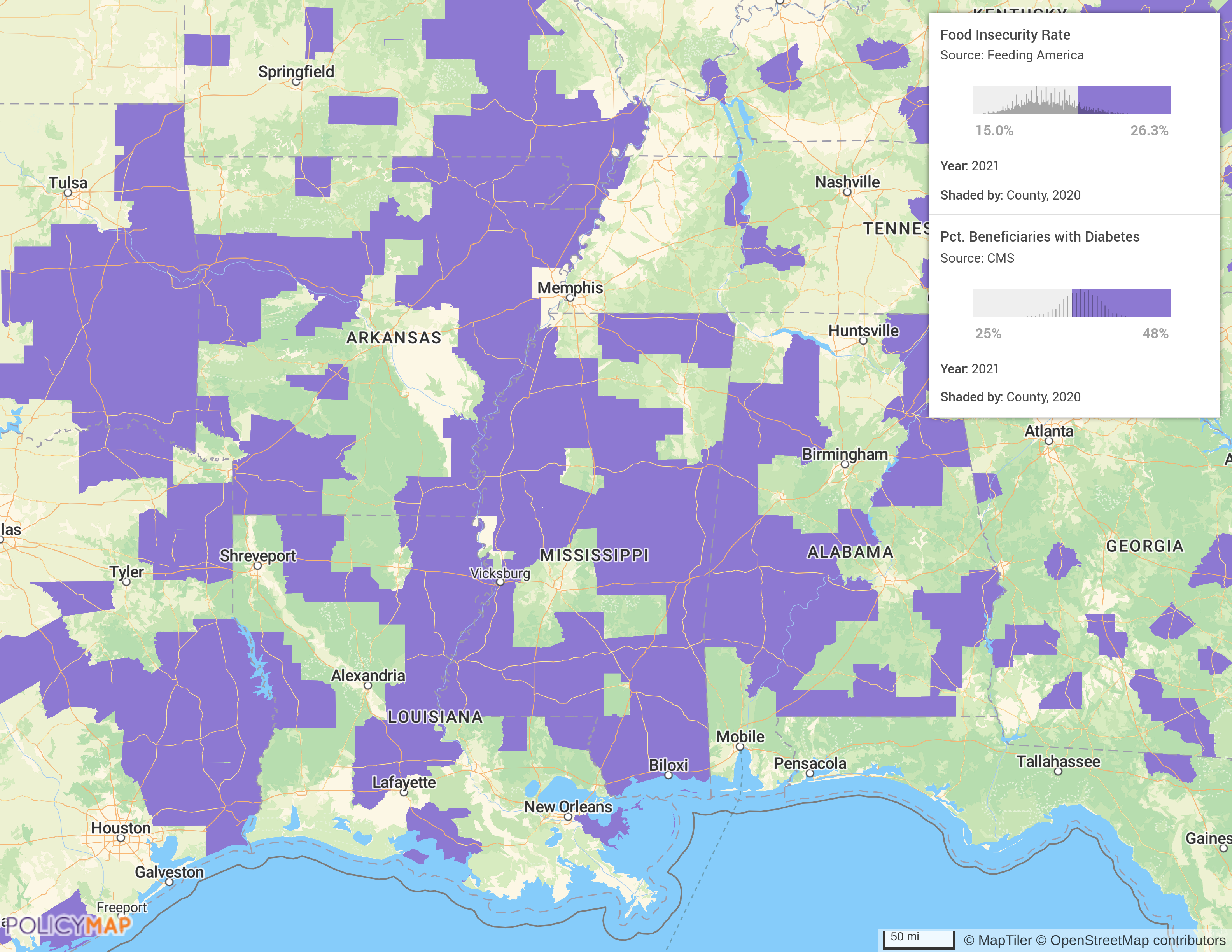
Users can also create a multi-layer map to deliver insights at the nexus of risk factors. The following map displays the prevalence of food insecurity and the percent of medicare beneficiaries with diabetes, according to data from the Centers for Medicare & Medicaid Services. PolicyMap has datasets on a wide variety of chronic conditions that can deliver insights on SDOH. This spatial analysis could allow public health officials, community organizations, or FaM startups to identify communities that would benefit from nutrition-centered interventions and medically tailored meals.
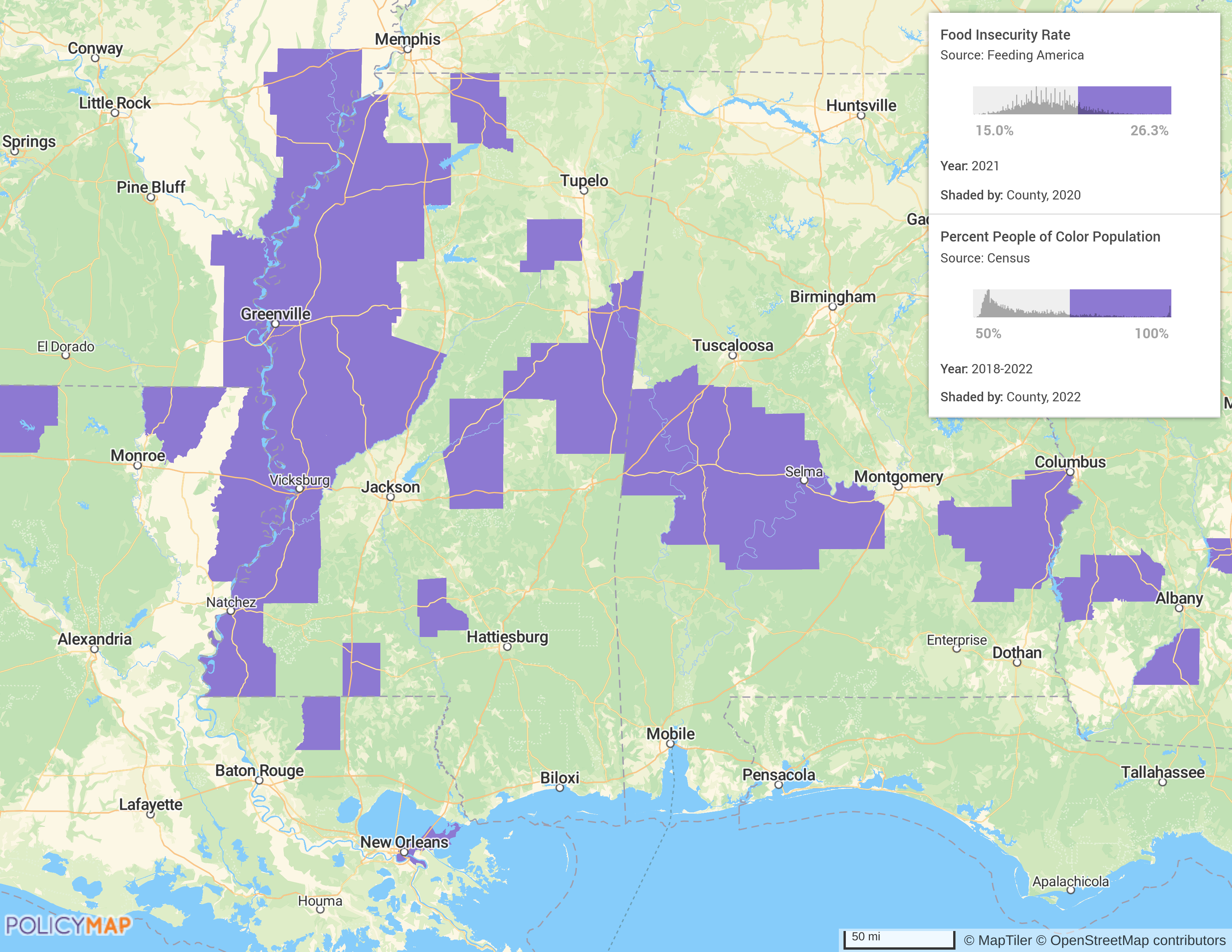
Food as medicine stands to benefit everyone, but certain groups face greater adversity in access to healthy food, the delivery of healthcare, and exposure to health risks. PolicyMap’s demographic data and metrics on food insecurity by county, visualized below by a multi-layer map, reveal the prevalence of health inequities in counties with a majority population of people of color.
Challenges & Opportunities in the FaM Landscape
The onset of thought-leadership on and funding for food as medicine initiatives is an opportunity for a variety of stakeholders to deliver organizational growth and improve community well-being. SNAP and WIC can incorporate FaM research to enable low-income families and disinvested communities to obtain nutritious food options. Instacart has already made the leap, as it currently accepts EBT and SNAP benefits from eligible users for online orders made to qualified grocery stores. Consumer-oriented platforms specializing in produce-prescriptions and medically tailored meals should also employ public health benefits to ensure equitable access across communities.
FaM-oriented non-profit organizations, already supported by foundations like the Rockefeller Foundation, can leverage insights on community health needs, nutrition education, and other barriers to entry to reach previously excluded, high-need populations. Building coalitions across sectors will be critical to ensure that healthcare and food-centered interventions are delivered equitably and cost-effectively.
Another group of stakeholders in the conversation about FaM are the payers, providers, and managed care organizations that support funding for health interventions. Medicare Advantage Supplemental Benefits and Section 1115 Demonstrations through Medicaid both offer incentives for participation in FaM models, advancing goals beyond traditional benefits. Commercially-funded payer mechanisms also serve a major role in supporting FaM access through payer claims and employer contracts, making up nearly 40% of FaM enterprise business models.
The Aspen Institute’s “Food-is-Medicine Research Action Plan,” a 100-page report designed to give a holistic view of the FaM space, identifies 18 recommendations for research design, collaboration, and equitable progress. The 12th recommendation, falling under the category of “metrics to advance clinical and policy decision-making,” delineates that “Researchers and experts from the fields of health care, nutrition, public health, and dietetics, as well as FaM providers and advocacy organizations, should identify a set of meaningful metrics that can be incorporated across Food is Medicine research design and evaluation.” The challenge with FaM comes down to making sense of data and properly identifying community-level needs.
The FaM landscape is experiencing substantial expansion and innovation, driven by government programs, commercial ventures, and evolving payer strategies. Integrating food-based interventions into healthcare will allow stakeholders to address diet-related diseases, reduce healthcare costs, and improve community health outcomes. Utilizing data-driven geospatial insights into SDOH allows initiatives to effectively serve individuals and communities. PolicyMap equips stakeholders with the tools to better understand and address issues like food insecurity, nutritional distress, government assistance enrollment, and a variety of critical health factors. This approach facilitates the optimal allocation of resources to meet nutritional needs, ensure program impact, and improve public health outcomes.
Request More Information
For more information on how PolicyMap can support your Food as Medicine initiatives, or to explore customized data solutions for addressing social determinants of health, please contact us using the form below. A member of our team will be in touch shortly.